Background:
RSV is a prevalent cause of acute lower respiratory infections, primarily in young children, but can also lead to severe pneumonia in adults, especially the elderly and immunocompromised. Hematological malignancies, a group of neoplastic disorders affecting blood, bone marrow, and lymph nodes, can render patients more susceptible to infections and complications. The aim of this study is to evaluate the impact of hematological malignancies on inpatient mortality, hospital length of stay, and hospitalization costs and charges in adult patients during RSV-related hospitalizations, using retrospective data from the National Inpatient Sample (NIS) 2020.
Methods:
In this retrospective cohort study, we used NIS data for 2020. International Classification of Diseases, Tenth Revision, with Clinical Modification (ICD-10-CM) codes were utilized to query the NIS database and identify adults (Age ≥18 years) hospitalized with RSV pneumonia. Our population of interest was subsequently divided into two groups based on the presence or absence of unremitted hematological malignancies.
Inpatient mortality served as the primary outcome, with secondary outcomes being hospital length of stay, hospitalization charges, and costs. A multivariate logistic regression analysis was conducted using STATA MP 16.1, incorporating various hospital and patient-level factors. The Charlson comorbidity index was utilized to account for the burden of comorbidities in the analysis.
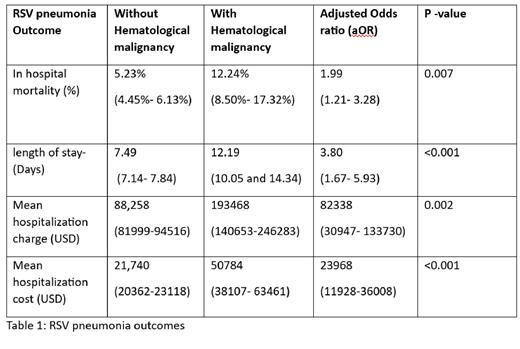
Results:
The total population of adult patients admitted in 2020 with RSV pneumonia was 13,900. From this, 980 individuals (7.1%) were diagnosed with a hematological malignancy, of which 43% were female. Conversely, 93% of individuals did not have a hematological malignancy, and, females accounted for 59% of this group. Patients with a hematological malignancy had a mean age of 66, while those without had a mean age of 69. In comparison to those without hematological malignancy, patients with this malignancy demonstrated a higher all-cause inpatient mortality rate for PSV pneumonia (12.24% versus 5.23%). When hospital and patient-level factors were taken into consideration, it was noted that RSV pneumonia patients with hematologic malignancy had a higher odds of all-cause inpatient mortality, with an adjusted odds ratio (aOR) of 1.99 (95% Confidence Interval (CI) 1.21- 3.28). Moreover, these patients had a longer hospital stay (12.2 days) compared to those without hematological malignancy (7.5 days), which reflects an adjusted mean difference of 3.8 days (95% CI 1.7-1.9). Overall, patients with hematological malignancies incurred higher mean hospitalization charges and costs, with an adjusted mean difference of USD 29,044 (95% CI 11,928 - 36,008) and USD 105,210 (95% CI 30,947 - 133,730), respectively.
Clinical Implications:
This study highlights the increased risk of inpatient mortality and resource utilization in RSV-related hospitalizations for patients with hematological malignancies. These findings emphasize the need for timely detection, prophylaxis, preference for antiviral treatment, and the inclusion of the RSV pneumonia vaccine in the prevention strategy. The results also inform healthcare administrators and policymakers about the importance of effective infection control measures, resource allocation, and public health initiatives to protect this vulnerable population.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal